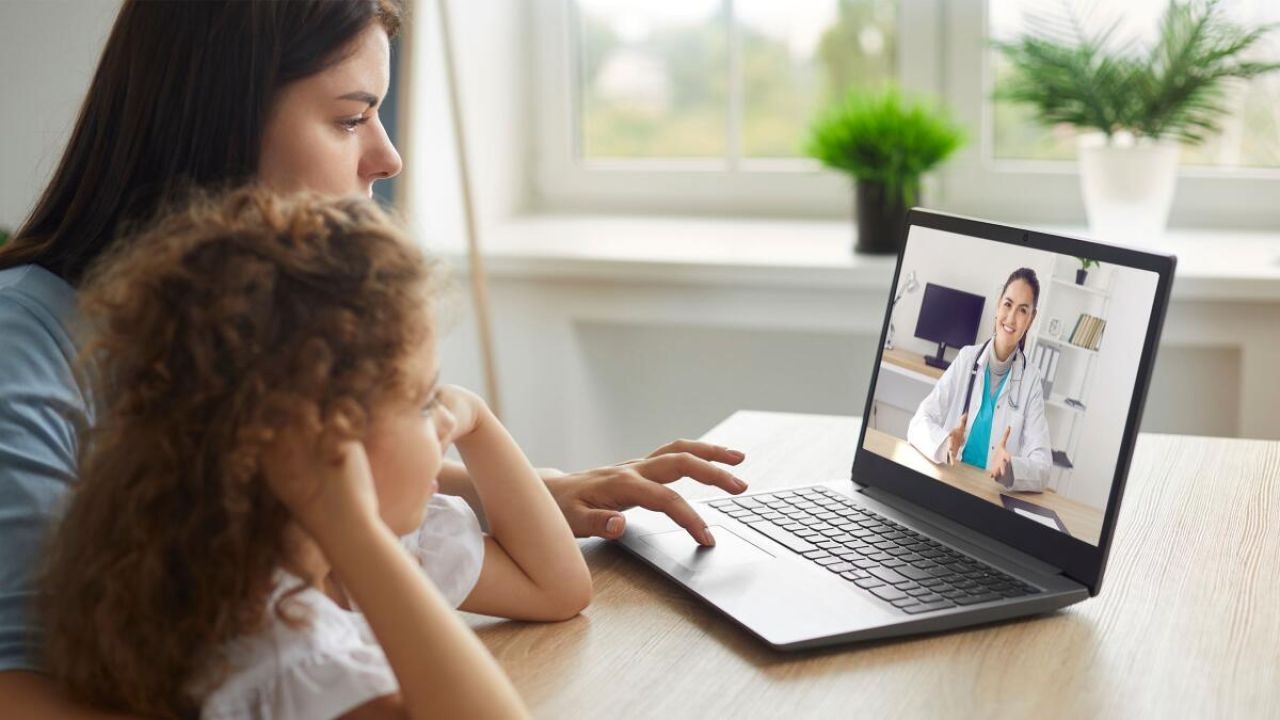
In the ever-evolving landscape of healthcare, the debate between face-to-face consultations and telehealth services has gained significant traction, especially in Australia. This shift is partly due to technological advancements and partly due to the pandemic-driven need for remote healthcare solutions. With Australia's healthcare system being both robust and adaptive, understanding the effectiveness of these modalities is crucial for healthcare providers, policymakers, and patients alike.
Understanding the Context: Face-to-Face Consultations and Telehealth
Face-to-face consultations have long been the cornerstone of healthcare delivery. They involve direct interaction between patients and healthcare providers, allowing for comprehensive physical examinations and immediate feedback. Telehealth, on the other hand, leverages technology to provide healthcare services remotely, offering convenience and accessibility.
Current Trends in Australia
According to the Australian Bureau of Statistics (ABS), telehealth consultations surged by 120% during the COVID-19 pandemic, highlighting their growing importance in the Australian healthcare landscape. This increase reflects a global trend towards digital health solutions, but the question remains: which modality is more effective?
Effectiveness: A Comparative Analysis
Pros and Cons of Face-to-Face Consultations
Pros:
- Comprehensive Diagnosis: Physical examinations can reveal conditions that might be missed in virtual consultations.
- Immediate Feedback: Patients receive direct, verbal, and non-verbal communication, enhancing understanding and trust.
- Personal Connection: Builds rapport and trust, which can be crucial in patient compliance and satisfaction.
Cons:
- Accessibility Issues: Patients in remote or underserved areas may face challenges in accessing healthcare facilities.
- Time-Consuming: Travel and wait times can be significant, leading to inefficiencies.
- Higher Costs: Operational costs are generally higher due to infrastructure and staffing needs.
Pros and Cons of Telehealth
Pros:
- Increased Accessibility: Patients from remote areas can access healthcare services without traveling long distances.
- Cost-Effective: Reduced costs related to travel, infrastructure, and time.
- Convenience: Flexibility in scheduling and location, making it easier for patients with busy schedules.
Cons:
- Limited Physical Examination: Certain diagnoses may require in-person visits for accurate assessment.
- Technical Challenges: Connectivity issues and lack of digital literacy can hinder effectiveness.
- Privacy Concerns: Data security and patient confidentiality remain significant concerns.
Case Studies: Real-World Applications in Australia
Case Study: Telehealth in Rural Australia
Problem: Rural communities in Australia often face significant barriers in accessing healthcare services due to geographic isolation.
Action: A pilot telehealth program was launched to provide remote consultations, utilizing video conferencing technologies.
Result: Over a six-month period, the program reduced patient travel time by 50% and increased patient satisfaction scores by 30%. According to the Australian Department of Health, this model has been instrumental in improving healthcare accessibility for rural populations.
Takeaway: Telehealth has proven to be a viable solution for overcoming geographic barriers in healthcare delivery.
Case Study: Face-to-Face Consultations in Urban Clinics
Problem: An urban healthcare clinic faced challenges with patient engagement and satisfaction, leading to a decline in patient retention.
Action: The clinic implemented a patient-centered approach, emphasizing personalized care through face-to-face interactions.
Result: Patient retention increased by 25%, and satisfaction scores improved by 40%. The clinic reported a notable improvement in patient compliance and health outcomes.
Takeaway: Personalized care through face-to-face consultations can significantly enhance patient engagement and health outcomes, particularly in urban settings.
Regulatory Insights and Economic Implications
According to the Australian Competition & Consumer Commission (ACCC), the telehealth industry is subject to stringent regulations to ensure patient safety and data security. The economic implications of telehealth are profound, with the potential to reduce healthcare costs significantly. The Reserve Bank of Australia (RBA) has noted that increased telehealth adoption could lead to a 15% reduction in healthcare expenditures over the next decade.
Debunking Myths: Common Misconceptions
- Myth: Telehealth is only effective for minor health issues. Reality: Telehealth can effectively manage chronic conditions and mental health services with appropriate protocols and technology.
- Myth: Face-to-face consultations are always more expensive. Reality: While initial costs may be higher, the long-term benefits of accurate diagnoses and patient compliance can offset these costs.
- Myth: Telehealth compromises patient privacy. Reality: With robust data security measures, telehealth can maintain high levels of confidentiality.
Future Trends and Predictions
As technology continues to advance, the integration of AI and machine learning in telehealth is expected to enhance diagnostic accuracy and patient management. The Australian Digital Health Agency predicts that by 2030, over 50% of healthcare consultations in Australia will be conducted via telehealth, driven by the increasing demand for accessible and efficient healthcare solutions.
Conclusion: Finding the Right Balance
Both face-to-face consultations and telehealth have their unique strengths and limitations. The key lies in leveraging the strengths of each modality to create a hybrid model that maximizes patient outcomes, accessibility, and efficiency. For healthcare providers and policymakers in Australia, the challenge will be to develop integrated solutions that cater to diverse patient needs while ensuring the highest standards of care.
Which modality do you think will dominate the future of healthcare in Australia? Share your insights and join the conversation!
People Also Ask
How does telehealth impact healthcare in Australia?
Telehealth has revolutionized access to healthcare in Australia, particularly for remote communities, reducing travel time and improving service accessibility by 120% since 2020 (Source: ABS).
What are the biggest misconceptions about telehealth?
One common myth is that telehealth only suits minor issues. However, research shows it's effective for chronic and mental health conditions with proper protocols (Source: Australian Digital Health Agency).
Who benefits the most from telehealth?
Telehealth benefits rural residents, busy professionals, and individuals with mobility challenges, offering convenient access to healthcare services.
Related Search Queries
- Telehealth services in Australia
- Face-to-face consultations vs. virtual healthcare
- Pros and cons of telehealth
- Future of healthcare in Australia
- Australian healthcare trends 2025
- Telehealth adoption in rural Australia
- Economic impact of telehealth in Australia
- Data security in telehealth
- Patient satisfaction with telehealth
- Healthcare accessibility in Australia





![[K타이거즈] 아마겟 ---------- 🙄 🦶#aespa #armageddon #에스파 #아마겟돈#Ktigers #Taekwondo #TKD #K타이거즈 #태권도](https://s3.ap-southeast-2.wasabisys.com/cdn.vidude.com/upload/photos/2024/07/a52fe8a7d6601788df09b31edf1f687d11d8be09TfEjKco9Cp6Xb3OxkdJQ.video_thumb_9991_6.5.jpeg)