New Zealand’s healthcare system, often praised for its public funding and accessibility, faces growing strains. With rising wait times and an aging population, many Kiwis are asking: Is private health insurance worth the cost? This article examines the trade-offs, trends, and tough choices facing households.
New Zealand’s healthcare system has long been a source of national pride. Built on the principle of universal access, it promises care based on need rather than ability to pay. Yet for a growing number of Kiwis, the question of whether public healthcare alone is enough has become increasingly pressing. Rising wait times, workforce shortages, and an ageing population are reshaping how people experience the system day to day. Against this backdrop, private health insurance is no longer viewed solely as a luxury. For many households, it is being reconsidered as a form of risk management rather than an upgrade.
This shift is not driven by ideology. It is driven by lived experience. The decision to take out private cover in New Zealand now sits at the intersection of public system capacity, personal health risk, income stability, and expectations about timeliness and choice.
How New Zealand’s public healthcare system actually works
New Zealand’s public health system is funded primarily through general taxation and administered nationally through Te Whatu Ora. In principle, it provides free or heavily subsidised hospital care, emergency services, and many specialist treatments. General practice visits, however, often involve co-payments, and access to allied health services can vary widely by region.
One of the system’s defining features is prioritisation. Elective procedures are assessed using clinical thresholds that determine who receives publicly funded treatment and when. This model is designed to allocate finite resources fairly, but it also means that access is shaped by capacity as much as need. For patients who fall below the threshold or face long delays, the system can feel less universal in practice than it does on paper.
Where pressure is building
Over the past decade, demand for healthcare services in New Zealand has increased faster than capacity in several key areas. An ageing population has led to higher rates of chronic illness and more complex care needs. At the same time, workforce shortages, particularly among nurses and specialists, have constrained service delivery. These pressures are unevenly distributed, with some regions experiencing significantly longer wait times than others.
For many Kiwis, the most visible impact is in elective care. Procedures such as orthopaedic surgery, cardiac interventions, and certain diagnostics can involve lengthy waits in the public system. While urgent and life-threatening conditions are prioritised appropriately, conditions that affect quality of life rather than survival often sit in a grey zone. This is where private health insurance tends to enter the conversation.
What private health insurance actually offers in New Zealand
Private health insurance in New Zealand does not replace the public system. Instead, it operates alongside it, offering access to private hospitals, faster diagnostics, and greater choice of specialist. Most policies focus on elective surgery and specialist consultations rather than emergency care, which remains predominantly public.
The value proposition is therefore not about better clinical outcomes in an absolute sense. New Zealand’s clinicians work across both systems, and standards of care are broadly comparable. The difference lies in timing, choice, and predictability. For people who can afford it, private cover can reduce uncertainty and allow treatment to be scheduled around work, family, and personal circumstances.
Who is most likely to benefit from private cover
Data from insurers and health researchers suggest that uptake of private health insurance is highest among middle- to higher-income households, older adults, and those with stable employment. These groups are more likely to face conditions where waiting time has a material impact on quality of life and earning capacity.
Self-employed individuals often view private cover as a form of income protection, reducing the risk that a delayed procedure could disrupt their livelihood. Parents may see it as a way to ensure timely care for children, particularly for conditions that sit outside acute emergency pathways. For these groups, the perceived benefit is not preferential treatment, but certainty in an otherwise uncertain system.
The cost side of the equation
Private health insurance in New Zealand is not inexpensive, and premiums tend to rise with age. This creates a tension that experts frequently debate. Insurance is most affordable when people are younger and healthier, but its perceived value often increases later in life when costs are highest.
This dynamic raises questions about equity and accessibility. Lower-income households are less likely to hold private cover, even though they may face greater barriers to navigating long public wait times. From a system perspective, this reinforces a two-track experience that sits uneasily with New Zealand’s egalitarian self-image, even if clinical outcomes remain broadly similar.
Common misconceptions about private insurance
One persistent misconception is that having private health insurance guarantees faster care in all circumstances. In reality, private capacity is also constrained, particularly in smaller centres. Another is that private insurance undermines the public system. The relationship is more complex. Private care can reduce demand on public hospitals for certain procedures, but it also draws clinicians from the same workforce pool.
There is also confusion about coverage. Many policies exclude pre-existing conditions or involve significant excesses. Without careful reading, some policyholders discover that the scenarios they most worried about are not fully covered. This has fuelled scepticism and, in some cases, dissatisfaction with the private insurance model.
Government policy and the absence of a clear stance
Unlike some comparable countries, New Zealand has never articulated a clear policy position on the role of private health insurance. It is neither actively promoted nor discouraged. Tax incentives are limited, and regulation focuses on consumer protection rather than system integration.
This neutrality reflects political sensitivity. Public healthcare remains a core part of New Zealand’s social contract, and overt encouragement of private insurance risks being interpreted as an admission of public system failure. At the same time, policymakers recognise that private provision is already embedded in the system, particularly for elective care. The result is a pragmatic but somewhat ambiguous coexistence.
What experts actually disagree on
Health economists and policy analysts broadly agree that private health insurance does not solve systemic capacity issues on its own. Where they differ is on its net effect. Some argue that it provides a pressure valve, allowing those who can afford private care to step out of public queues, indirectly benefiting others. Others caution that it entrenches inequality and diverts attention from necessary investment in public capacity.
There is also debate about long-term sustainability. As the population ages, reliance on private cover may increase, but so will premiums. Whether this model remains viable without broader reform is an open question.
The lived experience behind the numbers
Beyond policy and economics, decisions about health insurance are deeply personal. Many Kiwis take out private cover after a specific experience, such as a long wait for surgery or a delayed diagnosis. Others drop cover after years of paying premiums without making a claim. These stories shape public perception as much as any dataset.
What emerges from these experiences is not a clear verdict, but a pattern. Private insurance is rarely about seeking superior care. It is about managing time, stress, and uncertainty in a system under strain.
The NZ Healthcare Landscape: Public System vs. Private Insurance
New Zealand’s public healthcare system, funded through taxes, provides free or subsidized care for citizens and residents. Key pillars include:
Public Hospitals: Free emergency and essential treatments.
Pharmac: Subsidizes prescription medications.
ACC: Covers injury-related care, regardless of fault.
However, elective surgeries (e.g., hip replacements, cataract surgery) often face long waitlists. In 2023, over 35,000 people waited longer than four months for procedures, per Te Whatu Ora (Health NZ).
Private health insurance covers 28% of Kiwis (1.4 million people), according to the Health Funds Association (HFANZ). Policies typically fund faster access to specialists, elective surgeries, and private hospital rooms.
Why Consider Private Insurance? The Benefits
Shorter Wait Times:
Elective Surgery: Average public waitlist: 120+ days vs. 14–28 days privately.
Diagnostics: MRI scans in public hospitals face 6–8 week delays; private clinics offer next-day bookings.
Choice and Comfort:
Select specialists, avoid overcrowded public wards.
Coverage Gaps:
Public funding excludes many dental, vision, and mental health services.
“Insurance is a safety net for non-urgent care,” says Dr. Samantha Murton, President of the Royal NZ College of GPs. “For chronic conditions or cancer, it can literally save lives.”
The Drawbacks: Costs, Inequality, and Underinsurance
Soaring Premiums:
Average annual cost: NZ2,000–4,000 per person (HFANZ 2023).
Premiums rise sharply with age (e.g., 60+ pay 3x more than 30-year-olds).
Two-Tier System Risks:
Wealthier patients “jump the queue,” worsening public system strain.
Policy Exclusions:
Pre-existing conditions often excluded for 3–5 years.
“Private insurance isn’t a magic fix,” warns health economist Dr. Rhema Vaithianathan. “It fragments care and leaves lower-income families reliant on an overstretched public system.”
Global Comparisons: How NZ Stacks Up
Australia: 44% have private hospital cover (incentivized by tax penalties).
UK: 11% use private care despite free NHS access.
Canada: Private insurance banned for core services; NZ’s mixed model is more flexible but less equitable.
NZ’s hybrid system ranks 13th globally (Commonwealth Fund 2021) but lags in mental health and dental coverage.
Psychological Toll: Anxiety vs. Assurance
A 2023 NZ Health Survey found:
32% delayed GP visits due to costs (even with subsidies).
41% with private insurance cited “peace of mind” as their top reason.
Low-income families face “stress double-binds”: Pay premiums or risk waitlist limbo.
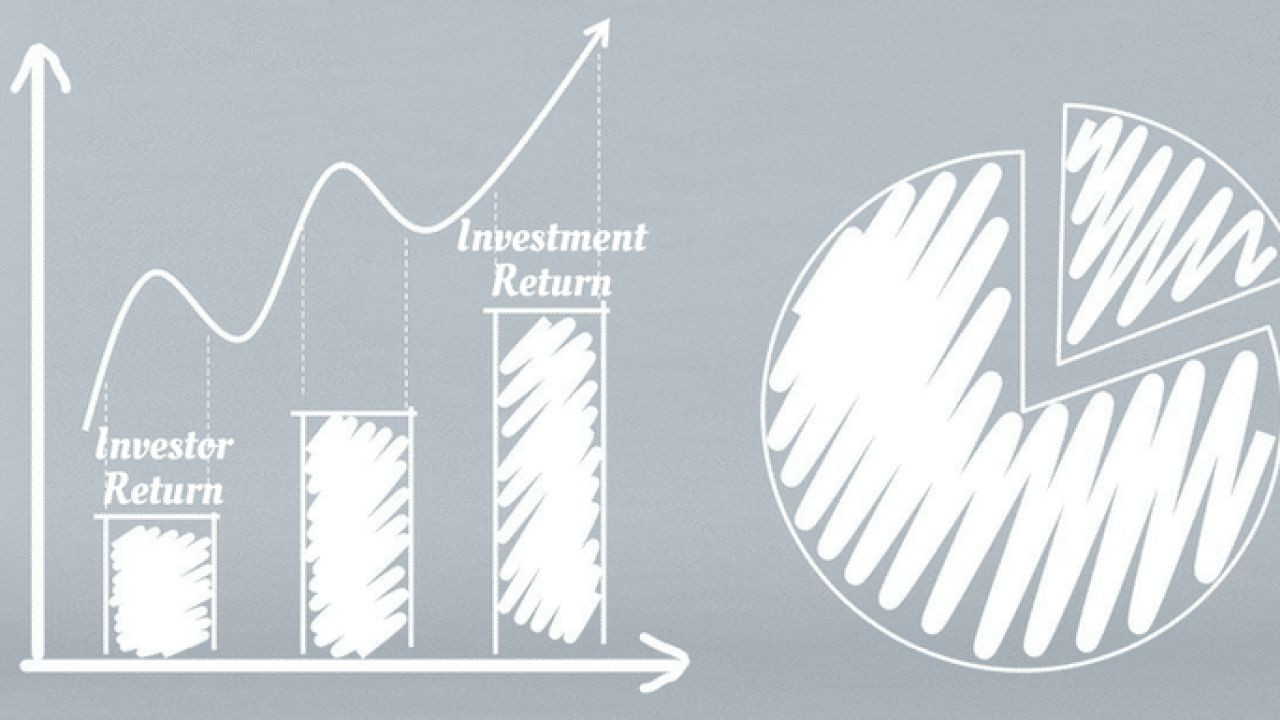
Predictive Modeling: A System Under Siege
By 2040, NZ’s elderly population will double, increasing demand for hip/knee surgeries and cancer care. Without reforms, Deloitte forecasts:
Public waitlists growing 5% annually.
Private premiums rising 8% yearly (outpacing wages).
Case Study: A Family’s Dilemma
The Smiths (mid-40s, two kids) pay NZ$450/month for private cover. When their son needed tonsil surgery:
Public path: 8-month waitlist.
Private path: Surgery in 3 weeks.
But… “We’re debating dropping coverage as premiums eat into our budget,” Mrs. Smith admits.
Expert Recommendations: To Buy or Not to Buy?
For Households:
Under 35, healthy? Prioritize ACC and save for out-of-pocket costs.
Families/Older Adults? Consider insurance if chronic conditions run in the family.
Compare policies: Use sites like MoneyHub to avoid overpaying.
For Policymakers:
Cap premium increases for older Kiwis.
Expand public dental and mental health funding.
Integrate private hospitals into public networks during crises.
What the next three to five years may bring
Looking ahead, pressures on New Zealand’s healthcare system are unlikely to ease quickly. Demographic trends, workforce challenges, and fiscal constraints suggest continued strain on public capacity. This may lead to incremental growth in private insurance uptake, particularly among working-age adults.
At the same time, there is increasing public conversation about how to strengthen the public system, including workforce investment and service redesign. The balance between public provision and private supplementation will remain contested, but it is unlikely to disappear.
For individual Kiwis, the decision to hold private health insurance will continue to depend on personal circumstances rather than ideology. The more relevant question may not be whether private cover is necessary in principle, but under what conditions it provides genuine value in New Zealand’s evolving healthcare landscape.
In that sense, private health insurance is neither a panacea nor a betrayal of public healthcare ideals. It is a pragmatic response to real constraints, shaped by data, experience, and the enduring expectation that access to care should be timely, fair, and humane.
The Verdict: A Personal Calculation
Private insurance offers speed and choice but at a steep price. For many, it’s a luxury; for others, a lifeline. As public waitlists grow, the question isn’t just “Can you afford insurance?” but “Can you afford NOT to have it?”
加入讨论 (Join the Conversation)
Have you used private insurance in NZ? Was it worth the cost? Share your story, debate solutions, and demand fairer healthcare access. Your experience could guide others facing this critical choice.
Engage & Act: Struggling to navigate NZ’s healthcare maze? Comment below, share this article, or tag policymakers to voice your concerns. Together, we can heal the system.



























scottybender4
12 months ago