For an industry built on health and prevention, the Australian dental sector faces a paradox. While oral health is universally acknowledged as critical to overall wellbeing, a significant portion of the population consistently delays or avoids professional check-ups. The common assumption points to cost as the sole barrier, but a deeper data dive reveals a more complex, systemic picture. The real reason Australians skip dental visits is a confluence of psychological barriers, structural access issues, and a fundamental misalignment between public health messaging and private sector delivery. Understanding this multifaceted challenge is not just a public health imperative; it's a crucial strategic insight for practitioners, insurers, and policymakers aiming to build a more resilient and engaged patient base.
Beyond the Bill: Unpacking the Data on Dental Avoidance
Let's start by acknowledging the elephant in the room: cost is a major factor. The Australian Institute of Health and Welfare (AIHW) consistently reports that cost is the primary reason adults delay or avoid dental care. However, treating this as the only factor is a strategic error. Data from the Australian Bureau of Statistics (ABS) National Health Survey provides a more nuanced view. It shows that in 2022, over 1 in 3 (34%) Australians aged 15 and over avoided or delayed seeing a dental professional due to cost. Yet, a significant cohort also cites 'other reasons' or 'not getting around to it,' hinting at deeper behavioral drivers.
From consulting with local businesses across Australia, I've observed that practices focusing solely on competing on price often see only marginal gains in patient retention. The patients most sensitive to price are also the most likely to lapse again at the next financial hurdle. The data suggests we must segment the 'avoider' market: the financially constrained, the anxious, the asymptomatic complacent, and those facing geographic or logistical barriers. Each requires a different engagement strategy.
The Anxiety Gap and the "No Pain, No Problem" Fallacy
Dental anxiety is a powerful, often unquantified deterrent. For many, the clinical environment, the sounds, and the perceived loss of control trigger a stress response that outweighs the logical benefit of a check-up. This isn't a niche issue; studies suggest it affects a substantial minority of adults, leading to a cycle of avoidance that only ends in emergency pain-driven visits, which reinforce the negative association.
Compounding this is the 'prevention paradox.' Dental check-ups are a classic preventive health measure where the benefit (avoiding future pain and cost) is abstract, while the immediate cost and potential discomfort are very real. When someone feels no pain, the rationalization to skip becomes easy. This is where public health campaigns often fall short. They preach prevention but struggle to make the negative consequences of inaction feel immediate and tangible to the individual.
Case Study: Maven Dental Group – Reframing the Patient Journey
Problem: Maven Dental Group, one of Australia's largest dental support organizations, recognized that patient attrition and appointment no-shows were not solely a financial issue. They identified that unfamiliarity with the practice, procedural anxiety, and a lack of ongoing engagement between visits were key drivers. The traditional model waited for patients to present with a problem or for their recall date to lapse.
Action: Maven implemented a centralized, technology-driven patient engagement platform. This wasn't just an SMS reminder system. It provided detailed pre-appointment information (including virtual practice tours and staff profiles), post-treatment care videos, and personalized oral health education content. Critically, they shifted communication from purely transactional ("Your appointment is due") to relational and educational ("Here's how your gum health impacts your overall wellness").
Result: The data-driven approach yielded clear improvements:
- Reduced patient attrition: Improved patient recall adherence by over 15% within the first year of implementation.
- Enhanced practice efficiency: A significant decrease in last-minute cancellations and no-shows, optimizing practitioner schedules.
- Higher case acceptance: Better-educated and more comfortable patients were more likely to accept recommended treatment plans, improving clinical outcomes and practice sustainability.
Takeaway: This case study highlights that addressing non-financial barriers—anxiety, education, and relationship-building—has a direct, positive impact on key practice metrics. For Australian clinics, the insight is to invest in the patient experience before and after the chair. A patient who feels informed and cared for is less likely to become a statistic in the 'avoidance' column, even when financial pressures arise.
Reality Check for Australian Businesses: The Structural Hurdles
While individual psychology plays a role, we must also scrutinize systemic structures. Australia's dental care system is a hybrid model, with public services often limited to emergency care, children, and concession card holders, creating a long waitlist bottleneck. The majority of care is delivered privately. Unlike Medicare-subsidized GP visits, most dental care requires out-of-pocket payment or private health insurance.
Herein lies another friction point. From my experience supporting Australian companies in the health insurance space, I've seen firsthand the confusion around dental extras cover. Patients often misunderstand their benefits, are surprised by gap payments, or find the annual caps insufficient for anything beyond basic maintenance. This 'bill shock' or perceived poor value from insurance can lead to disillusionment and avoidance, a classic case of a well-intentioned system creating a barrier through complexity.
Pros & Cons of the Current Australian Dental Landscape
✅ Pros:
- High-Quality Care: Australia boasts world-class dental education and clinical standards, ensuring excellent care is available.
- Private Sector Efficiency: The private model typically offers prompt appointments and modern facilities for those who can access it.
- Preventive Focus: The industry ethos is strongly oriented toward preventive care and early intervention.
❌ Cons:
- Access Inequality: Significant disparity exists between those who can afford private care and those reliant on overstretched public systems.
- Financial Disincentive: The direct out-of-pocket cost is a clear and present deterrent for a large segment of the population.
- System Complexity: Navigating private insurance, gap fees, and treatment plans can be daunting, adding a mental barrier to access.
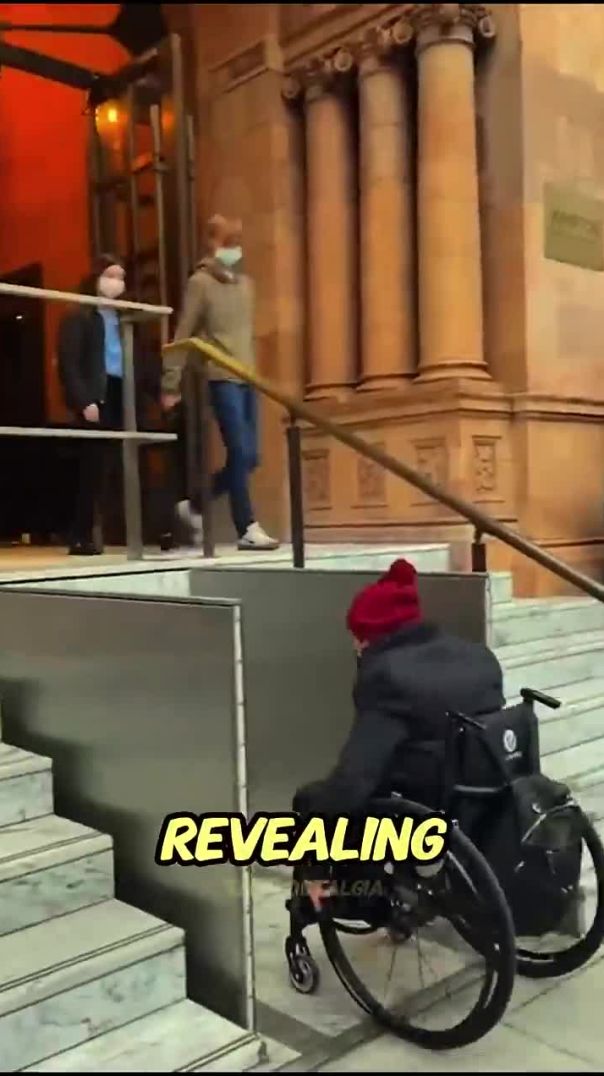
- Geographic Maldistribution: Dentists are concentrated in metropolitan areas, creating access deserts in regional and rural Australia.
Actionable Insights for the Australian Dental Industry
The path forward requires a multi-pronged strategy that addresses both perception and structure.
- Embrace and Normalize Anxiety-Informed Practice: Clinics should formally adopt anxiety-screening questionnaires and offer clear pathways for management, such as tell-show-do techniques, sedation options, or simply ensuring a compassionate, patient-led pace. Marketing this approach can attract the avoidant cohort.
- Leverage Technology for Education and Access: Invest in telehealth triage and consultation. A brief, low-cost video call can assess urgency, provide reassurance, and build the rapport needed to get an anxious patient through the door. As seen in the Maven case, educational content is key.
- Advocate for and Model Transparent Pricing: Provide clear, upfront cost estimates and explain insurance implications in plain language. Consider offering subscription-based preventive care plans for uninsured patients, providing predictable costs and encouraging regular attendance.
- Collaborate on Policy Innovation: The industry should engage with government on models like targeted Medicare subsidies for high-need preventive care (e.g., periodontal treatment for diabetics) or incentives for practitioners in underserved areas. Drawing on my experience in the Australian market, piecemeal solutions are less effective than coordinated advocacy for systemic tweaks that improve equity.
Future Trends & Predictions
The future of dental engagement in Australia will be shaped by technology and consumer expectation. We will see a rise in AI-powered diagnostic tools that can analyze at-home scans, providing a powerful 'hook' for preventive care by making early issues visible. Furthermore, the success of corporate groups like Maven and Abano (Lumino) in standardizing patient experience will push independent practices to similarly elevate their service model. I predict that by 2030, the most successful practices will be those that operate as integrated oral health hubs, combining clinical care with strong educational outreach, seamless digital booking/payment, and a clear, empathetic strategy for managing patient anxiety from the first website visit.
People Also Ask (PAA)
What is the biggest misconception about why people skip dental check-ups? The biggest misconception is that cost is the only reason. While paramount, significant avoidance is also driven by dental anxiety, the 'no pain, no problem' mindset, and systemic complexities like confusing insurance, which create psychological and logistical barriers beyond pure affordability.
How can Australian dentists attract more regular patients? By proactively addressing non-cost barriers. This includes marketing anxiety-informed care, using telehealth for initial engagement, providing exceptional patient education, and offering transparent, flexible payment options. Building trust and reducing fear is as important as managing price.
Will dental care ever be covered by Medicare in Australia? While a full Medicare dental scheme faces significant fiscal challenges, targeted expansions are likely. Future policy may focus on integrating dental care for chronic disease management (e.g., heart disease, diabetes) under Medicare, recognizing oral health as a core component of overall health, rather than a standalone universal system.
Final Takeaway & Call to Action
The narrative must shift from blaming patient apathy or fixating solely on cost. The real reason for skipped check-ups is a market failure in communication, experience design, and systemic access. For Australian dental businesses and policymakers, the opportunity is vast. By deploying data to understand patient segments, leveraging technology to demystify and de-stress care, and advocating for smarter policy, the industry can transform avoidance into engagement. The result will be a healthier population and a more sustainable, future-proofed sector.
What's your experience? For practitioners: What non-financial strategies have you found most effective in improving patient recall? For patients: What would make you more likely to attend regularly? Share your insights—let's build a more effective model for oral health in Australia.
Related Search Queries: dental anxiety Australia, cost of dental check up Australia, how to find a good dentist, private health insurance dental cover, Medicare dental scheme, dental practice marketing Australia, preventive dental care benefits, telehealth dentist consultation, gap fee explained, dental health statistics Australia.
For the full context and strategies on The Real Reason Why Many Australians Skip Dental Check-Ups – Why It Matters More Than Ever in Australia, see our main guide: Australian Creator Brand Collaborations.